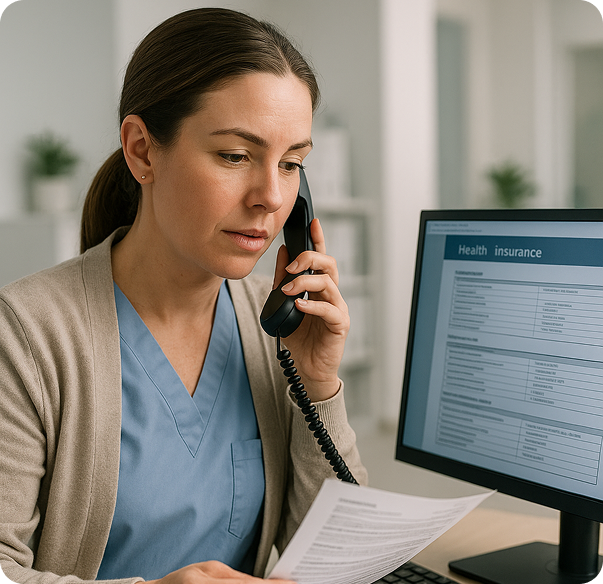
Stop Denials Before They Happen with Proactive Insurance Verification
The single most effective way to improve your clean claim rate is to verify patient eligibility before the appointment. Our insurance verification services do exactly that, saving you time, money, and frustration.
Up to 75% of claim denials are caused by front-end issues like incorrect patient information or inactive coverage. When you discover a patient’s insurance is invalid after you’ve provided a service, you are left with an unexpected denial and a difficult financial conversation. This erodes revenue and damages the patient relationship.
Pre-Appointment Check
24-48 hours before the scheduled visit, we check the patient’s insurance status with the payer.
Comprehensive Detail-Check
We don't just see if the policy is "active." We confirm co-pays, deductibles (and how much has been met), co-insurance percentages, and any pre-authorization or referral requirements.
Alerts and Updates
We immediately alert your front-desk staff to any issues, allowing them to collect the correct co-pay or resolve the insurance problem with the patient before they are seen.
- Drastically Reduce Denials - Prevent claim denials related to eligibility, the most common reason for rejection.
- Improve Upfront Collections - Collect the correct co-pay and deductible amounts every single time.
- Enhance Patient Experience - Patients appreciate knowing their financial responsibility upfront, avoiding surprise bills.
- Increase Staff Efficiency - Your front desk can focus on patient care, not on fixing billing errors.